In Memoriam
Patrick “Pat” Brophy
Remembering Patrick “Pat” Brophy, a transformational leader, whose focus was always on the children. Patrick (“Pat”) D. Brophy, MD, MHCDS, beloved husband, father, brother, friend, and leader, left us all…
Read MoreArant, Billy S., Jr.
Arant, Billy S., Jr. Pediatric Nephrologist Collected Antique Furniture And Rare Books Billy S. Arant, Jr., M.D. of Chattanooga died on September 12, 2023, after a long illness. He…
Read MoreJohn Stewart Cameron
John Stewart Cameron BSc (1956) MRCS LRCP (1959) MB BS (1959) MRCP (1961) MD (1964) FRCP (1971) CBE (1998) 05 July 1934 – 30 July 2023 We are…
Read MoreTribute to Adrian Spitzer: A Visionary in Developmental Nephrology
Adrian Spitzer (born December 21, 1927; passed December 27, 2021), past President, American Society of Pediatric Nephrology, was from Bucharest, Romania, and graduated from the Carol Davila University of Medicine…
Read MoreBruce A. Kaiser, MD
It is with great sadness we announce that Bruce A. Kaiser died after a brief illness on December 3, 2021 in Medford NJ, his hometown of 38 years. Bruce is…
Read MoreSusan E. Thomas, MD
Dr. Susan E Thomas, M.D., former Associate Professor of Pediatrics, passed away in early April after a lifetime of managing Cystinosis. She completed medical school at Loyola University Chicago Stritch…
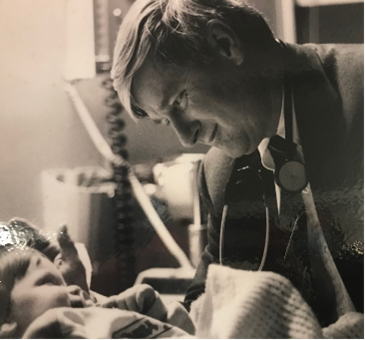
Read MoreWilliam E. “Bill” Segar
Bill Segar died peacefully at home, in Indianapolis, IN on Feb 1, 2021. He was 97 years old. A very touching tribute to him was written by his son Jeff…
Read MoreH. William Schnaper Tribute Page
Life Course Journey of a True Mensch H. William (Bill) Schnaper was the Irene Heinz Green & John LaPorte Given Chair in Pediatric Research and Tenured Professor & Vice Chair,…
Read MoreJohn Herrin (2020)
It is with great sadness that we announce the passing on October 25, 2020 of John T. Herrin, MBBS, FRACP, 84, former Director of Clinical Services within the Division of Nephrology at Boston…
Read MoreMichel Broyer (2020)
We are very sad to announce the death of Professor Michel Broyer on March 10, 2020 at the age of 86, following a COVID19 infection. Early during his residency in…
Read More